Study identifies potential pathway to reducing breast cancer brain metastases
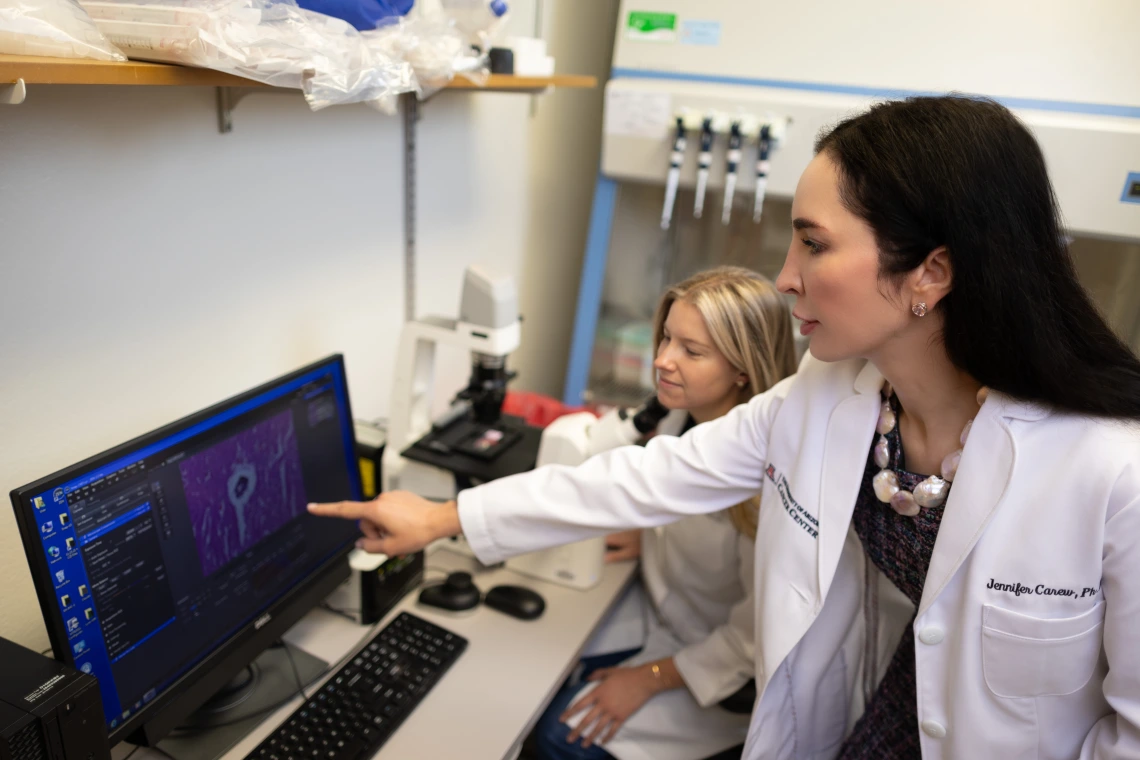
Dr. Jennifer Carew works with a student in her lab at the University of Arizona Cancer Center.
A study led by researchers from the University of Arizona Cancer Center at UArizona Health Sciences identified a biological mechanism that could lead to more effective treatments for breast cancer that has metastasized to the brain.
By studying the metabolic differences between primary breast cancer cells and those that metastasize to the brain, they determined that autophagy was significantly upregulated in brain metastases. Autophagy is a cellular recycling process that cancer cells can use to stay alive when faced with stressful conditions such as those triggered by anticancer drugs.
“The prognosis for individuals with brain metastases from breast cancer is extremely unfavorable, and the management of breast cancer metastases in the brain remains a formidable challenge,” said senior author Jennifer Carew, PhD. “We were able to disrupt breast cancer cells’ ability to form brain metastases by impairing the autophagy pathway.”
In the study published in Clinical and Translational Medicine, the researchers first showed that targeting the key autophagy regulating gene ATG7 significantly reduced the ability of breast cancer cells to form brain metastases in mouse models.
With the goal of developing a strategy to bring this discovery to patients, the research team investigated whether hydroxychloroquine, a Food and Drug Administration-approved drug, could potentially be used to treat breast cancer brain metastases. Hydroxychloroquine inhibits autophagy at a later point in the pathway and, importantly, readily crosses the blood-brain barrier.
“Most drugs do not efficiently cross the blood-brain barrier, and that is one of the key reasons why brain metastases are so difficult to treat,” said Carew, who is a professor of medicine at the UArizona College of Medicine – Tucson and a member of the UArizona Cancer Center Clinical and Translational Oncology Program.
The research team combined hydroxychloroquine with lapatinib, which is FDA-approved to treat breast cancer. They showed that this drug combination successfully reduced the number and size of breast cancer brain metastases in mouse models.
Hydroxychloroquine has been combined with a number of other anticancer agents in early phase clinical trials, but this is the first time researchers have studied its effectiveness when combined with lapatinib for breast cancer therapy.
Carew said the team was amazed by how significantly they were able to diminish the ability of breast cancer cells to form brain metastases by targeting a single pathway.
“Cancer cells, unfortunately, have evolved so many ways that make it difficult for us to stop their growth or kill them,” Carew said. “It is always somewhat surprising when you see how changing only one thing can have an impact.”

Drs. Steffan Nawrocki, left, and Jennifer Carew talk in their lab in the University of Arizona Cancer Center.
“Our group and others have shown that activation of autophagy makes it harder for many different types of cancer therapies to kill cancer cells and this promotes drug resistance,” said first author Steffan Nawrocki, PhD, co-director of the Cancer Center Clinical and Translational Oncology Program and professor in the UArizona College of Medicine – Tucson. “Because hydroxychloroquine and lapatinib are already FDA approved, we can advance this drug combination quickly into a clinical trial for patients with breast cancer brain metastases.”
Brain metastases are the most prevalent adult central nervous system tumors, with 20% to 30% of cases resulting from breast cancer patients, particularly those with triple negative and HER2 amplified disease. Managing breast cancer metastases in the brain is challenging, with only 20% of patients with breast cancer brain metastases surviving beyond five years.
Growing successes
The team has successfully developed multiple clinical trials based on the novel therapeutics research in their lab and hope to do that once again with this study.
“We will be working with Dr. Jennifer Segar, one of our breast cancer medical oncologists here at UACC, to design a clinical trial that will evaluate autophagy inhibition as a strategy to prevent the development of brain metastases in women with breast cancer who are at high risk to develop them as well as to treat patients with existing brain metastases,” Carew said.
Segar is also an associate professor of medicine in the University of Arizona College of Medicine. Carew said this second goal in collaboration with Segar is particularly important because patients with brain metastases are excluded from participating in most clinical trials due to neurological symptoms that are caused by their brain tumors.
“These patients continue to have a huge unmet need that we are excited to address by developing our own clinical trial where we write the ‘rules’ defining who is eligible to participate,” she said.
The researchers also have a very active autophagy-focused drug discovery program. The first novel autophagy inhibitor that they invented, called ROC-325, has been licensed for clinical development.
A researcher works in the lab of Drs. Steffan Nawrocki and Jennifer Carew.
“We are currently creating newer inhibitors that are even more potent and hope to take them into clinical trials here at UACC when they are ready,” Dr. Carew said.
Other co-authors include Wei Wang, PhD, professor in the R. Ken Coit College of Pharmacy; former doctoral student Trace M. Jones, PhD; Claudia M. Espitia, assistant staff scientist in the College of Medicine – Tucson; postdoctoral fellow Maria Janina Carrera Espinoza, PhD; and doctoral students Madison E. Gamble, Sruthi Sureshkumar and Mengyang Chang.
This research was supported by the National Cancer Institute, a division of the National Institutes of Health, under Award Nos. T32CA009213, R21CA184649, R01CA190789, R01CA268383 and P30CA023074.



