Too Much of a Good Thing: Managing Immunotherapy Side Effects
Immunotherapy can backfire when a supercharged immune system attacks healthy cells, but researchers are hopeful for the future.
by Anna C. Christensen, UA Cancer Center
Originally published in the Spring 2018 issue of Act Against Cancer
 One of the most attractive features of immunotherapies like checkpoint inhibitors is that they teach immune cells to target cancer specifically, setting them apart from chemotherapy and radiation, whose attacks on tumors spill over onto healthy cells. But if immunotherapy ignores healthy cells while waging war on cancer cells, the unpleasantness associated with chemotherapy and radiation shouldn’t be an issue.
One of the most attractive features of immunotherapies like checkpoint inhibitors is that they teach immune cells to target cancer specifically, setting them apart from chemotherapy and radiation, whose attacks on tumors spill over onto healthy cells. But if immunotherapy ignores healthy cells while waging war on cancer cells, the unpleasantness associated with chemotherapy and radiation shouldn’t be an issue.
“Side effects tend to be relatively minor,” says Emmanuel Katsanis, MD, University of Arizona Cancer Center division chief of pediatric hematology and oncology. “Patients don’t lose their hair, they don’t have nausea and vomiting, they don’t get mouth sores. Most of it can be done as an outpatient.”
Despite immunotherapy’s well-earned reputation as a kinder, gentler cancer treatment, in a small percentage of patients it can have serious side effects. Sometimes, immune cells become hypervigilant and start attacking healthy cells, a phenomenon known as autoimmunity.
“In the same way that an activated immune system is attacking the cancer, immunotherapy may cause similar side effects, as you would see in autoimmune conditions like lupus or rheumatoid arthritis,” says Dr. Katsanis.
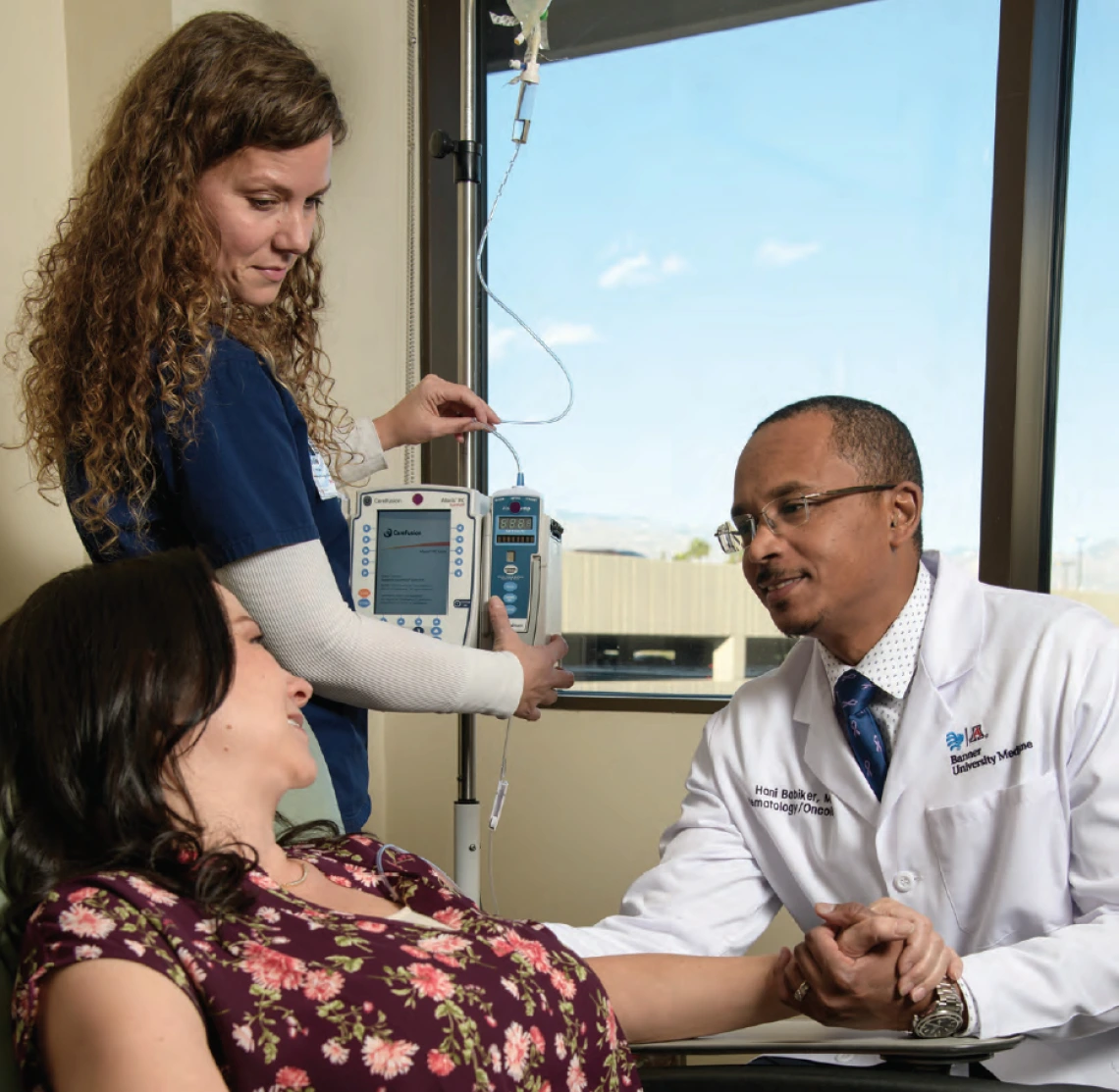
“If you awaken the immune system to fight cancer, sometimes those armies of immune cells could attack ‘self,’” says Hani Babiker, MD, associate director of the UA Cancer Center Early Phase Clinical Trials Program. Fortunately, autoimmune side effects are rare. “Not a lot of patients get side effects. I would dare say that serious side effects are less than 8 percent of patients, in some of the drugs.”
Furthermore, most side effects are mild and do not interfere with a patient’s day-to-day life.

Rousing the immune system: A range of side effects
Daniel Persky, MD, director of the UA Cancer Center Clinical Trials Office, says many types of immunotherapies, especially monoclonal antibodies, carry a risk of an allergy-like reaction to the infusions.
“We’re very well prepared for such side effects because we’ve had a lot of experience dealing with these drugs,” says Dr. Persky. “We typically give medications beforehand, such as Benadryl and Tylenol. We may give a corticosteroid like prednisone to reduce the possibility of a reaction.”
Fortunately, allergic reactions to infusions usually pose no long-term problems.
“Typically, after a person has been exposed to it, the body gets used to the drug,” says Dr. Persky. “The subsequent risk of similar infusion reactions is much less.”
Beyond the initial possibility of reacting to the infusion of the drugs, side effects can accompany treatment. Rashes or itching are common, but they can be treated effectively with topical medicines like corticosteroid creams or antihistamines.
Other side effects, however, are similar to those experienced by people receiving chemotherapy, including fatigue, which is the No. 1 side effect experienced by patients using checkpoint inhibitors.
 “Fatigue, the most common side effect, is not debilitating and it’s better tolerated with time,” says Daruka Mahadevan, MD, PhD, director of the UA Cancer Center Early Phase Clinical Trials Program.
“Fatigue, the most common side effect, is not debilitating and it’s better tolerated with time,” says Daruka Mahadevan, MD, PhD, director of the UA Cancer Center Early Phase Clinical Trials Program.
Additionally, whereas chemotherapy can directly attack healthy cells in the gastrointestinal tract, so too can immunotherapy deploy over-revved immune cells to this region of the body, resulting in similar side effects, such as difficulty eating, nausea and diarrhea.
Fortunately, severe side effects from immunotherapy are rare.
“In my practice, the side effects we see with immunotherapy are much less than what we see with chemotherapy,” says Dr. Babiker.
The most serious side effects are linked to uncontrolled inflammation — conditions that end in the suffix –itis, like pneumonitis, colitis or hepatitis. Although inflammation is a normal part of the immune response, in which the body fights against injuries, infections or cancers, there can be too much of a good thing. Chronic inflammation can harm healthy tissue, potentially leading to major damage. Fortunately, UA Cancer Center physicians know what to look out for.
“We keep a close eye on all side effects,” says Dr. Mahadevan of his clinical trial patients. Members of his staff “contact trial patients frequently to see how they’re doing. We bring them in regularly for check-ups so we don’t miss anything.”
Ultimately, if a patient’s cancer goes into remission, these side effects might be worth it. “I’d rather have a patient who’s alive with some autoimmune symptoms than a cancer that metastasizes and kills the patient,” says Dr. Katsanis.

Fighting fire with fire: Addressing side effects with medication and education
When the immune system is hyperactive, it needs to be tamed, and UA Cancer Center physicians have the necessary tools.
 “We have learned a lot about how to manage these side effects over the course of the last decade,” says Julie Bauman, MD, MPH, UA Cancer Center division chief of hematology and oncology.
“We have learned a lot about how to manage these side effects over the course of the last decade,” says Julie Bauman, MD, MPH, UA Cancer Center division chief of hematology and oncology.
The trick is to strike a balance between letting the immune system kill cancer cells, while suppressing it just enough to bring autoimmune conditions under control. A class of drugs called corticosteroids frequently is used to counter immunotherapy side effects.
Outside the field of oncology, health-care providers are gaining awareness of the unique side effects immunotherapy can trigger. If a cancer patient visits the emergency department with shortness of breath and a cough, a physician more familiar with the immune-suppressing effects of chemo, rather than the immune-enhancing effects of immunotherapy, might diagnose the patient with an infection and prescribe antibiotics — but what if the patient actually has a life- threatening case of autoimmune pneumonitis?
“When a person comes to the ER with a severe infection, the time to antibiotics is critical,” Dr. Bauman says. “Similarly, if a person comes to the ER with severe autoimmune side effects, it’s the time to steroids that really matters.”
To provide appropriate treatment, health-care providers must be able to distinguish between infections and autoimmune symptoms.
“There is a clear need to educate first responders, urgent care centers and emergency departments to recognize autoimmune responses,” says Dr. Bauman, who has helped educate other health-care providers about immunotherapy, whether addressing colleagues at conferences or talking to other physicians one on one. “If I have a patient who’s going to an ER, I call the ER physician directly and let them know what they need to be looking for, and teach them about immunotherapy,” says Dr. Bauman. “They are so appreciative, because it really is a completely new treatment.”

The road ahead: Improving the patient experience
All medical treatments have side effects, and immunotherapy is no exception. It is tempting to hope that the side effects associated with surgery, radiation and chemotherapy can be left in the past, with immunotherapy raising armies of perfectly trained immune cells to target tumors and leave innocent bystanders alone. But the power of the immune system can be a double-edged sword. Fortunately, scientists and physicians are learning how to wield it.
By continuing to unravel the mysteries of the immune system, researchers hope in the near future we will make strides in identifying appropriate biomarkers — chemicals in the body that can be measured to give doctors information about what is going on inside, perhaps by blood tests or molecular tumor testing. These biomarkers could help us predict which patients are more likely to respond to an immunotherapy — and who might be at risk for serious side effects.
“Identifying the biomarkers for response to immunotherapy can help us select specific immunotherapeutic drugs, one over the other, to fight specific cancers,” says Dr. Babiker.
Researchers at the UA Cancer Center are investigating a new method to identify biomarkers in a simple skin biopsy, which might be used to predict which patients will have serious side effects to a drug. In the future, tests that uncover information about a tumor’s biomarkers or genetics could help physicians match individual patients to the safest and most effective drugs.
“We have the ability to sequence the human genome, and we have a multitude of immunotherapy candidates,” says Dr. Bauman. “When these two things come together, we will have powerful cancer therapy for every person. We can wake up their immune system to the unique antigens within their cancer. That is the holy grail.”



