Hepato-pancreato-biliary: gastric resection
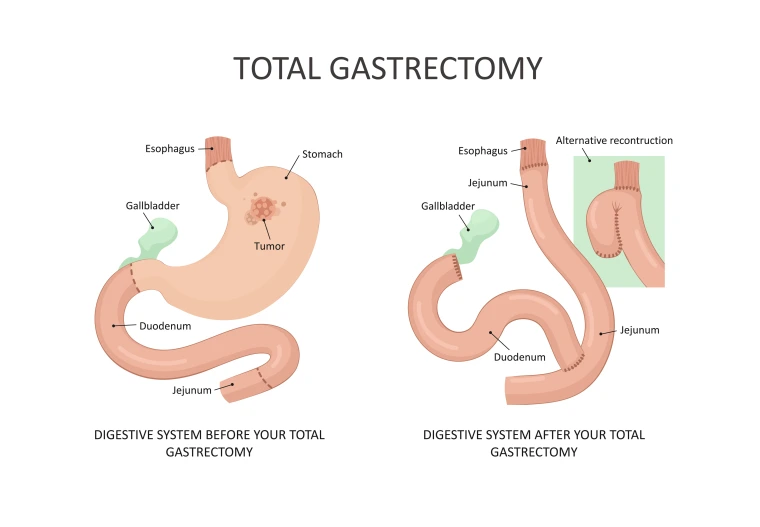
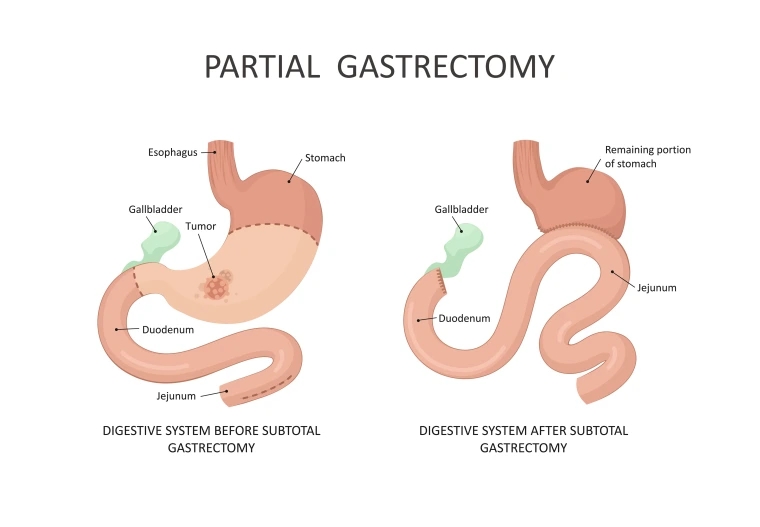
Stomach resection surgery may be done for a number of different reasons. It may be used to treat problems such as ulcers or bleeding, however, it is most commonly recommended for patients who have been diagnosed with stomach cancer. Based on the location of the stomach, different resections are performed from removing part of the stomach (Partial gastrectomy) to the removal of the entire stomach ( Total gastrectomy).
Total gastrectomy
Gastric resection information
Anastomotic leak – when there is a leak at the new attachment sites
Anastomotic stricture- when there is narrowing at the new attachment sites
Bile reflux – when bile flows back into the stomach and/or esophagus causing abdominal pain
Dumping syndrome- when food travels to your small intestine before it’s been broken down enough. This can cause unpleasant symptoms, including nausea, bloating, pain and diarrhea.
Deficiency in Iron, vitamin B12, which can result in anemia
Afferent and/or Efferent loop syndrome- when digestive juices that need to flow freely to help you break down food get trapped in your small intestine. It can cause symptoms like abdominal pain, nausea and vomiting
Bleeding
Infection, at the level of the wound, intra-abdominal, or bloodstream
Pain
Risks of anesthesia
Blood clot forming in your legs and lungs
Cardiopulmonary event- pneumonia, heart attack
Death
- Discuss with your surgeon your use of blood thinning medications such as Warfarin, Lovenox, Heparin, Pradaxa, Xarelto, Eliquis, ASA, Plavix, and other anticoagulants/antiplatelets.
- Exercise daily prior to surgery. Exercising will help your body get into its best condition for your surgery and make your recovery faster and easier.
- Do not wear any metal objects. Remove all jewelry, including body piercings. The equipment used during your surgery can cause burns if it touches metal.
- If you are a smoker, stopping smoking 4wks before surgery is strongly recommended to lower the risk for lung and wound complications.
- Shower with an antimicrobial soap the evening before and the morning of surgery. Please, do not shave the surgical area 48 hrs prior to surgery.
- The day before your surgery, you may eat a regular diet. Starting Midnight, you may only drink clear liquids ( sports drinks, tea, coffee without creamer or milk, apple juice, water, clear broth, popsicles). You can continue with a clear liquid diet until 2 hours prior to your surgery.
- 1-7days prior to your scheduled surgery, pre-anesthesia clinic will call you to review your medical history and medications as well as review pre-operative instructions. Pre anesthesia clinic number: 520-694-4232
- A surgery scheduler will call to confirm your surgery and arrival time by calling your phone number on file between 2 pm and 4pm the day prior to surgery. (For Monday surgeries, you will receive a call on Friday). Please, make sure to answer the call and check your voicemail. Scheduler number: 520-694-2873.
- The morning of surgery, you will check in at the admission desk on the first floor and register. They will send you up to the preoperative waiting room on the third floor once you are registered.
- Nurses and staff members will confirm your name, date of birth, procedure, and surgeon. This will be done multiple times, by multiple people during your stay to ensure your safety.
- You will then need to change into a surgical gown.
- Before surgery an IV line is put into a vein usually in your arm. This is used to inject fluids and medications into your veins as needed.
- While you are asleep, additional IV lines may be placed.
- While asleep we will insert a urinary catheter into your bladder. A nasogastric tube will also be placed extending from your nose into your stomach. Both of these tubes will be present when you awake
- Upon completion of the operation, your surgeon will place 1 drain into the abdominal cavity which will extend out through the skin and remain in place for the next few days. There are times when you need to go home with the drain in place. If this is the case, you will be shown how to care for it.
- The anesthesia team will block the nerves around your incision before you wake up to help with pain control after surgery.
After surgery you will be admitted to the hepatobiliary floor for recovery (9EW). You may need to go to the ICU in certain situations but most people do not need the ICU. The following outlines the expected daily progress, however, each patient is unique and daily progress may vary.
Day 0:
- You will receive pain medications, IV fluids, and lab work will be monitored daily.
- At all times while in bed, a Sequential Compression Devices (SCDs) will be wrapped around your legs and inflated with air. This helps prevent blood clots.
- You will also get blood thinner shots to help prevent blood clots. If you have cancer, you will go home with these shots for a total of 28days from time of surgery.
- You will have a tube in your nose (nasogastric tube); this tube is connected to wall suction. It helps suction fluid from your stomach and keep you from getting nauseated.
- You will have a urinary catheter which will drain urine from your bladder. This may make you feel like you need to urinate. This will be removed on postoperative day 1.
- Your goal is to sit on the side of your bed or up in chair at least one time on the day of your surgery.
- You will be given a breathing machine (Incentive Spirometer); you should use this 10 times every hour while you are awake. It is important to exercise your lungs so they expand fully, which can help prevent pneumonia. You can take this machine home with you.
- We will check your blood sugar every 6 hours.
Day 1:
- Nasogastric tube is removed; this can vary depending on your individual situation. It may stay in a day or two longer but is usually removed by 48-72 hours after surgery.
- Urinary catheter is removed.
- Ice chips are started.
- You will be asked to be out of bed in a chair all day and walk at least 4 time daily until discharge. Moving around and walking will help lower your risk for blood clots and pneumonia (lung infection). It will also help you start passing gas and having bowel movements again. Your nurse or physical therapist will help you move around, if needed.
Day 2:
- Your diet will be advanced to clear liquids if you are not nauseated or vomiting. When eating, you much be upright on a chair. Do not eat or drink while in bed/laying down. This may lead to aspiration.
- If you do vomit after the nasogastric tube is removed, it is possible that we might need to put it back in.
- Ambulation, Incentive Spirometer, eating only in an upright position will be encouraged daily.
Day 3:
- If you don’t have nausea or vomiting, your diet will be advanced each day at your surgeon’s discretion.
- Abdominal drains may be removed or decision may be made to keep the drains for a longer period of time.
Day 4-7
Discharge planning home or to a skilled rehabilitation facility per patient need.



