Catching a symptomless cancer early

Stephanie Worrell uses the best techniques, guidelines and people to improve patient results
What are the most common early warning signs of lung cancer? Actually, the answer is a surprising, there aren’t any.
“Lung cancer is tricky,” said Stephanie Worrell, MD, section chief for the Division of Thoracic Surgery at Banner University Medical Center, associate program director for the general surgery residency program and member of the U of A Cancer Center Thoracic Cancer Clinical Research Team.
“Most of the people who come to us are diagnosed incidentally, which means they went to the emergency room for a car accident or a shoulder problem, and they get imaging that found a lung nodule,” she said.
With no clear symptoms to alert them, thoracic surgeons like Worrell and her thoracic team rely on screening programs and robotic biopsies for early detection.
“Unfortunately, nationally, only about 6% of people who qualify for lung cancer screening actually get their screening CT scans,” Worrell said. “In Arizona, it's about 1.5% of people, so that's one of our big efforts this year. The five-year survival for lung cancer overall is still really poor.”
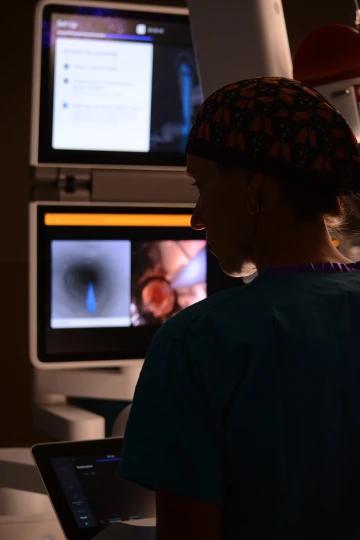
Stephanie Worrell, MD, checks a monitor in a surgery room at Banner Health in Tucson.
Lung cancer is the leading cause of cancer death in both men and women in the U.S., according to the National Cancer Institute. From 2009 to 2013, there were more deaths from lung cancer than colorectal, breast, prostate and liver combined. Though the overall survival rate for lung cancer is only 18%, patients have a better chance when it is detected early, and especially before it has spread elsewhere in the body.
To offer the best success for early screening patients, the cancer center and Banner Health are focusing their efforts on offering patients the latest technology with robotics and developing patient trials that offer the newest opportunities as early as possible.
“The robotics help us diagnose and find cancer in patients earlier,” Worrell said.
Recently, members of the Lung Nodule Program and Thoracic Oncology Program completed more than 300 biopsies in less than 14 months using the newest technological innovation––an Ion robotic bronchoscopy by Intuitive that allows for a minimally invasive peripheral lung biopsy.
These early-stage biopsies improve the amount of early-stage lung cancer being removed, according to Billie Bixby, MD, U of A clinical assistant professor and director of the Interventional Pulmonary Division of Pulmonary, Allergy, Critical Care and Sleep Medicine for Banner – University Medical Center in Tucson and Cancer Center associate member.
“This program is just getting started,” Bixby said. “We will have several more milestones as we change the landscape of the diagnosis and treatment of early and advanced lung cancer.”
Who should be screened for lung cancer?
People who qualify for lung cancer screening programs are 50 to 80 years old and have smoked a pack of cigarettes or more a day for 20 years and are current smokers or quit within 15 years.
“There are a lot of people at risk for lung cancer,” Worrell said. “We do know that there is an increasing instance of lung cancer in non-smokers, particularly women. Hopefully, we'll have some screening guidelines in the next couple of years to help pick up those people as well.”
The cancer center and Banner Health have a multidisciplinary tumor board for both lung and esophageal cancer as well as other malignancies that don't fall into those two categories.
“We really approach everything collaboratively for all patients. It's the pulmonologist, the radiologist, our medical and radiation oncologist that come up with a holistic plan for the patient,” she said. “I think that's really important to offer people the best chance at a cure or long-term survival by just getting multiple people's inputs and opinions.”
They also rely on patients who enroll in clinical trials to make progress with the disease and have recently opened two clinical trials in early lung cancer.
“Clinical trials at the cancer center help oncologists identify if patients need immunotherapy, targeted therapy with surgery or just earlier therapy,” she said. “Doing trials on early lung cancer will hopefully help us improve our outcomes.”
Bringing guidelines and innovations to all
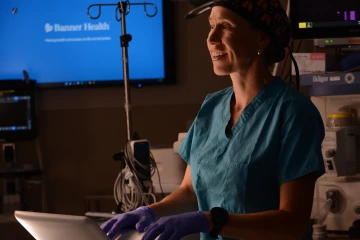
Stephanie Worrell, MD, demonstrates the ION an Ion robotic bronchoscopy by Intuitive that allows for a minimally invasive peripheral lung biopsy.
In addition to being a top-rated surgeon, Worrell brings with her a wealth of experience in working collaboratively to approach cancer for her patients, for the university and for the nation. She works with national colleagues as the chair of the esophageal cancer guidelines for the Society of Thoracic Surgeons.
Last year, Worrell also helped develop the first comprehensive guidelines for managing patients with thoracic esophageal cancer coauthored by the Society of Thoracic Surgeons, American Society for Radiation Oncology and American Society of Clinical Oncology, which outlines best practices for multidisciplinary management of esophageal cancer including contributions from medical and radiation oncologists and surgeons.
“The treatment right now is rapidly evolving, and so I think these guidelines will help inform people as far as treatment choices, when to treat, and when to operate,” she said.
Training the next generation of thoracic surgeons
The shelves in Worrell’s office are lined with photos of women thoracic surgeons, both colleagues and people she has mentored. These national and local mentoring relationships are important to her, and she is on the board of directors for the Women in Thoracic Surgery, a national organization where she also serves as mentorship chair.

Stephanie Worrell works with Jairo Martinez, a University of Arizona alum, demonstrating the ION robotic assisted bronchoscopy.
“Mentorship is really important to me because I've had a lot of really good mentors that have helped me get to where I am,” she said. “If you looked at all cardiothoracic surgeons, only about 7% are women. A lot of women don't have a mentor who is another woman, or they just don't even know that it's a career they could pursue. And so just showing people that it's possible, I think really will help increase that number so that we can look more like the general population.”
Worrell has been working to reformat the mentorship program with general surgery residents at Banner University Medical Center. It pairs residents with a faculty member and offers events every three months through their Cardiothoracic Surgery Fellowship and General Surgery Program for young thoracic and general surgeons.
Originally from Phoenix, Worrell said she is personally invested in southern Arizona, and her colleagues and patients in this community.
“I've always wanted to come back to Arizona––there's something special about the desert and working here,” she said. “Growing up, I loved the University of Arizona, and so I'm just happy to be back in a hometown environment and working here.”

